Diabetes Guide for Prevention and Management
The statistics are sobering: Diabetes UK estimates diabetes affects 5.6 million people in the UK, with hundreds of thousands living undiagnosed. As we mark World Diabetes Day, it's crucial to understand not just the condition itself, but how to prevent and manage it effectively.
Whether you're concerned about developing diabetes, recently diagnosed, or supporting someone with the condition, knowledge is your strongest ally. Recent studies suggest that with proper understanding and early intervention, many cases of Type 2 diabetes can be prevented or their onset delayed.
In this article, we'll explore the fundamentals of diabetes, share evidence-based prevention strategies, and discuss effective management techniques. You'll discover practical steps you can take today to reduce your risk and maintain better metabolic health.
Understanding Different Types of Diabetes
Diabetes occurs when your body struggles to process glucose effectively, leading to elevated blood sugar levels. According to Diabetes UK, cases have more than doubled in the past 15 years, making it one of the nation's most pressing health challenges.
Type 1 Diabetes:
- Affects approximately 400,000 people in the UK
- Autoimmune condition where the body attacks insulin-producing cells
- Usually develops in childhood or early adulthood
- Requires lifelong insulin therapy
- Cannot be prevented but can be effectively managed
Type 2 Diabetes:
- Affects over 4 million people in the UK
- Body becomes resistant to insulin or doesn't produce enough
- Can be prevented or delayed through lifestyle changes
- May require medication but can sometimes be managed through lifestyle alone
Risk Factors and Warning Signs
Common Risk Factors:
| Risk Factor | Type 1 | Type 2 |
| Genetics | Primary factor | Contributing factor |
| Age | Usually young | Usually over 40 |
| Weight | Not a factor | Significant factor |
| Lifestyle | Not a factor | Major factor |
| Ethnicity | Some influence | Strong influence |
Warning Signs to Watch For:
- Increased thirst and frequent urination
- Unexplained weight loss
- Extreme fatigue
- Blurred vision
- Slow-healing wounds
- Recurring infections
Diabetes Prevention and Management
While Type 1 diabetes cannot be prevented, you can significantly reduce your risk of Type 2 diabetes through:
Lifestyle Modifications:
Regular Exercise: Aim for at least 150 minutes of moderate activity weekly, spread across different days. This could include brisk walking, swimming, or cycling. Consider combining cardio with strength training exercises at least twice a week. Even small increases in physical activity, like taking the stairs or walking short distances, can make a significant difference.
Balanced Diet: Focus on a diet rich in vegetables, lean proteins, whole grains, and healthy fats. Include at least five portions of fruits and vegetables daily. Choose complex carbohydrates over simple sugars, as they release energy more slowly and help maintain stable blood sugar levels. Consider the Mediterranean diet pattern, which research shows can help prevent Type 2 diabetes.
Weight Management: Maintain a healthy BMI through a combination of proper nutrition and regular exercise. Even a modest weight loss of 5-10% can significantly reduce your risk of Type 2 diabetes. Work with healthcare professionals to set realistic weight goals and develop sustainable strategies to achieve them.
Sleep Quality: Prioritize getting 7-9 hours of quality sleep each night. Poor sleep can affect insulin sensitivity and increase cravings for sugary foods. Establish a regular sleep schedule, create a relaxing bedtime routine, and ensure your bedroom is dark, quiet, and cool for optimal rest.
Stress Management: Chronic stress can affect blood sugar levels and make it harder to maintain healthy habits. Incorporate stress-reducing activities into your daily routine, such as meditation, deep breathing exercises, yoga, or gentle stretching. Consider keeping a stress diary to identify and address triggers.
Alcohol Moderation: If you drink alcohol, do so in moderation. The NHS recommends not exceeding 14 units per week, spread over several days. Be aware that alcoholic drinks can be high in calories and affect blood sugar levels.
Regular Health Monitoring: Keep track of your health markers through regular check-ups. This includes monitoring your blood pressure, weight, blood sugar levels, and any symptoms you experience. Consider keeping a health diary to share with your healthcare provider.
Hydration: Drink plenty of water throughout the day. Proper hydration helps your body regulate blood sugar levels and supports overall metabolic function. Aim for 6-8 glasses daily, more if you're physically active or in warm weather.
Regular Monitoring:
- Blood glucose levels
- Blood pressure
- Cholesterol levels
- Kidney function
- Eye health
- Foot health
The Role of Professional Support
Managing diabetes effectively requires regular medical supervision and support. At CAS Medical, our Metabolic Health Assessment service provides:
- Comprehensive blood glucose testing
- Full lipid profile analysis
- Body composition assessment
- Personalised risk assessment
- Detailed dietary and lifestyle advice
- Regular monitoring and follow-up care
Our team of specialists works with you to:
- Identify early warning signs
- Develop personalised management plans
- Monitor progress effectively
- Adjust treatment as needed
- Prevent complications
- Support long-term health goals
Taking Action
Understanding your risk factors and current health status is the first step toward preventing or managing diabetes effectively. CAS Medical's Metabolic Health Assessment provides a thorough evaluation of your metabolic health and risk factors, along with personalised recommendations for prevention or management.
Don't wait for symptoms to appear. Contact CAS Medical today to schedule your Metabolic Health Assessment at our Glasgow, Bothwell, or Stirling clinics. Our experienced team will help you understand your risk factors and develop a tailored plan to maintain optimal metabolic health.
Early intervention and regular monitoring are key to preventing complications and maintaining quality of life. Take control of your metabolic health today – your future self will thank you.
To book your Metabolic Health Assessment or learn more about our diabetes management services, email info@casmedical.org
Your journey to better metabolic health starts here.
Navigating the Transition: Understanding Menopause
As a woman in your 40s or 50s, you're likely juggling a multitude of responsibilities - career, family, and personal growth. Amidst all this, your body is embarking on its own journey. From changes in memory, low energy, poor sleep, difficulty problem solving, aches and pains, and fatigue, to more classical symptoms of hot flushes, sweating and menstrual cycle changes. If these resonate with you, you might be entering the transformative phase of life known as menopause. Let's explore this natural transition together, shedding light on what menopause really means for you and your future.
The Menopause Metamorphosis: What's Really Happening?
For years, your hormones have been well balanced. But now, as you approach midlife, things are changing. This hormonal shift marks the beginning of perimenopause, the prelude to menopause. It's a time of change that can span several years, culminating in menopause itself - officially defined as the point when you've gone 12 consecutive months without a menstrual period.
According to the NHS, the average age for a woman to reach menopause in the UK is 51, but it can happen much earlier or later. In fact, about 1% of women experience premature menopause before the age of 40, according to the NHS.
The Stages of Menopause
Menopause unfolds in stages:
- Perimenopause: Usually beginning in your mid-40s. Your ovaries gradually produce less oestrogen, leading to irregular periods and the onset of menopausal symptoms.
- Menopause: Marking 12 months since your last period. At this point, your ovaries have stopped releasing eggs and are producing much less oestrogen.
- Postmenopause: Encompassing all the years after menopause. While some symptoms may ease, it's important to be aware of potential health risks associated with lower oestrogen levels.
Signs and Symptoms
Your body has its own unique way of communicating, and during menopause, it might feel like it's speaking a new language altogether. Here are some common experiences:
- Hot flushes and night sweats
- Irregular periods
- Mood changes
- Vaginal dryness
- Sleep disturbances
- Changes in libido
- Fatigue
- Joint and muscle aches
- Weight gain
- Hair loss
It's important to remember that these symptoms can vary greatly from woman to woman. Some might experience all of them, while others may have only a few or even none at all.
Strategies for Thriving with Menopause
While menopause is a natural part of ageing, you don't have to suffer through its symptoms in silence. Here are some strategies that many women find helpful:
- Lifestyle adjustments:
- Regular exercise (aim for at least 150 minutes of moderate exercise per week)
- Balanced diet rich in calcium and vitamin D
- Stress-reduction techniques like meditation or yoga
- Environmental modifications:
- Keeping your bedroom cool
- Dressing in layers to manage hot flushes
- Carrying a portable fan for sudden hot spells
- Medical interventions:
- Hormone Replacement Therapy (HRT)
- Non-hormonal medications for specific symptoms
- Topical hormone therapy for vaginal symptoms
- Alternative therapies:
- Some women find relief with treatments like acupuncture or tai chi
- Omega-3 fatty acids may help with night sweats
- While some tout the benefits of black cohosh or soy isoflavones, more research is needed to confirm their effectiveness
It's crucial to note that what works for one woman may not work for another. Your journey through menopause is as unique as you are. Consulting with a health specialist is important to help discover what will work for you.
Beyond the Transition: Looking to the Future
Menopause marks the end of your reproductive years, but it certainly doesn't signal the end of your vibrant life. Many women report feeling a renewed sense of freedom and confidence post-menopause. Without the monthly cycle to contend with, you might find new opportunities for travel, career advancement, or personal pursuits.
However, it's important to be aware of potential health considerations post-menopause, such as an increased risk of osteoporosis and cardiovascular disease. Regular check-ups, a healthy lifestyle, and discussions with your healthcare provider about preventive measures can help mitigate these risks.
Time to Take Control of Your Menopause Journey
As you navigate this midlife transition, remember that knowledge is power. Understanding what's happening in your body can help you make informed decisions about your health and wellbeing.
If you're feeling overwhelmed or unsure about your menopause symptoms, it's time to seek professional guidance. CAS Medical is here to support you through every stage of your menopause journey. With clinics in Glasgow, Bothwell, and Stirling, we offer accessible, personalised care tailored to your unique needs.
Don't let menopause catch you off guard. Book a consultation with CAS Medical today and take the first step towards embracing this new chapter of your life with confidence and vitality.
Breast Cancer Guide: Early Detection and Risk Factors
In the realm of women's health, breast cancer affects the lives of countless individuals and families. As we mark Breast Cancer Awareness Month, it's time to shine a light on this pervasive disease, arming ourselves with knowledge and the power of early detection. Unlike the occult nature of fibromyalgia we discussed previously, breast cancer presents a tangible threat that we can actively combat through awareness and vigilance.
In this article, you'll discover the crucial early signs of breast cancer that every woman should know. We'll explore how often you should be getting checked, demystify the process of self-examinations, and reveal when it's time to speak to a doctor. But that's not all - we have some surprising insights about risk factors that might change the way you think about your breast health.
The Silent Intruder: Understanding Breast Cancer
Breast cancer develops when abnormal cells in the breast begin to grow out of control, forming a tumour that can often be felt as a lump or seen on an x-ray. In Scotland, every year around 4,800 people are diagnosed with breast cancer, according to Breast Cancer Now. Cancer Research UK reports that 23% of UK breast cancer cases are preventable (2015). This gives hope for those with a breast cancer diagnosis.
Early Signs
Knowing the early signs of breast cancer is like having a secret language with your body. Here's what to look out for:
- A new lump or area of thickened tissue in either breast
- A change in the size or shape of one or both breasts
- Discharge from either nipple (which may be streaked with blood)
- A lump or swelling in either armpit
- Dimpling on the skin of your breasts
- A rash or skin change on or around your nipple
- A change in the appearance of your nipple, such as becoming sunken into your breast
Remember, these signs don't necessarily mean you have breast cancer, but they do warrant a conversation with your doctor.
Screening
Self-Examination
Performing regular breast self-exams is like having a monthly check-in with your body. Here's a simple guide:
- Visual Inspection:
- Stand in front of a mirror with your arms at your sides
- Look for any changes in breast size, shape, or skin texture
- Raise your arms and look for the same changes
- Manual Examination:
- Lie down and use your right hand to examine your left breast, then vice versa
- Use a firm, smooth touch with the first few finger pads of your hand
- Cover the entire breast from top to bottom, side to side—from your collarbone to the top of your abdomen, and from your armpit to your cleavage
- Nipple Check:
- Gently squeeze each nipple and check for discharge
Perform this self-exam once a month, about a week after your menstrual period ends. For those who don't menstruate, choose a day that's easy to remember, like the first of each month.
Mammogram Schedule
Just as you wouldn't skip regular maintenance for your car, you shouldn't neglect regular breast cancer screenings. In the UK, the NHS Breast Screening Programme automatically sends your first invite for breast screening between the ages of 50 and 53. Then you'll be invited every 3 years until you turn 71. Moreover, through private medical care, many women prefer not to wait until they are aged 50, and chose to undergo mammography breast screening earlier:
- Women 40-44: Consider yearly mammograms
- Women 45-54: Yearly mammograms
- Women 55 and older: Mammograms every 1-2 years, continuing as long as you're in good health
Remember, these are general guidelines. Your personal screening schedule should be discussed with your doctor, taking into account your individual risk factors.
Risk Factors: Breast Cancer Awareness
Understanding your risk factors for breast cancer is a roadmap for your health journey. While some factors, like age and family history, are beyond our control, others are lifestyle-related and can be modified:
| Non-Modifiable Risk Factors | Modifiable Risk Factors |
| Age (risk increases with age) | Alcohol consumption |
| Family history of breast cancer | Obesity |
| Dense breast tissue | Lack of physical activity |
| Early menstruation or late menopause | Hormone replacement therapy |
When to Speak to a Doctor: Trust Your Instincts
If you notice any changes in your breasts, don't wait. At CAS Medical, we believe that no concern is too small when it comes to your health. Led by Dr Chris Sockalingam, CAS Medical is here to listen, examine, and guide you through any worries you may have about your breast health.
At CAS Medical, we're not just private healthcare providers; we're your allies in the fight against breast cancer. Our services include:
- Comprehensive breast examinations
- Guidance on self-examination techniques
- Referrals for mammograms and other imaging studies
- Risk assessment and personalized screening plans
- Support and counselling throughout your breast health journey
With clinics in Bothwell, Glasgow, and Stirling, we're conveniently located to serve you and your family.
“Regular check-ups and early detection are the cornerstones of effective breast cancer prevention. They transform fear into empowerment, uncertainty into action. Remember, every moment spent on breast awareness is an investment in your future. Your vigilance today could be your victory tomorrow.”
Dr Chris Sockalingam
Taking Action: Your Health, Your Choice
Breast cancer awareness isn't just about wearing pink ribbons; it's about taking concrete steps to protect your health and encouraging others to do the same. By understanding the early signs, performing regular self-exams, adhering to screening schedules, and promptly addressing any concerns with a healthcare professional, you're taking control of your breast health and giving yourself the best chance of beating the disease.
Remember, early detection is your most powerful weapon against breast cancer. Don't let fear or busy schedules stand in the way of your health. According to a YouGov survey commissioned by Breast Cancer Now, only 53% of respondents in the UK said they’d report any new or unusual breast changes to their GP.
Schedule an appointment with CAS Medical today, and let's work together to keep you healthy and thriving. Your health is your most valuable asset. Invest in it wisely, starting with breast cancer awareness and prevention. After all, the life you save could be your own.
Types of Grief and How to Seek Support
Grief is like a shadow that falls across our lives, a deeply personal response to loss that can leave us feeling lost and overwhelmed. While it's an experience we all share at some point or another, grief is not simple, nor is it straightforward to deal with. It takes many forms, each as unique as the individual experiencing it.
In this article, we'll explore the various faces grief can assume. We’ll shed some light on how to find support when the weight of loss feels too heavy to bear alone. By understanding the different types of grief, we can better navigate this challenging emotional terrain and find our way forward towards lasting healing.
As we delve deeper into this topic, you might be surprised to learn about a form of grief that often goes unnoticed, silently affecting many people in their day-to-day lives. We'll uncover this hidden aspect of grief later in the article.
The Many Faces of Grief
As you will see below, grief isn't a one-size-fits-all emotion. It manifests in various ways, each with its own set of challenges, characteristics, and possible effects or impacts. Let's explore some common types of grief:
- Acute Grief: This is the raw, intense sorrow that washes over us immediately after a loss. It's like being caught in an emotional storm, where feelings of sadness, anger, and disbelief swirl around us. Characteristics include:
- A deep longing for the person or thing we've lost
- Difficulty accepting the reality of the loss
- Feeling emotionally numb or profoundly sad.
- Anticipatory Grief: Imagine knowing a storm is coming but you’re powerless to stop it. That's anticipatory grief - the mourning that occurs before an expected loss. Often experienced by those caring for terminally ill loved ones, it's a complex mix of dread, sorrow, and sometimes, guilty relief.
- Complicated Grief: When the initial storm of acute grief doesn't subside, it can sometimes evolve into a complicated type of grief. This persistent, intense form of grief can last for months or even years, making it difficult for the person experiencing it to move forward with regular life. It's like being stuck in a maze of sorrow, unable to find the exit. This constant reminiscing brings on waves of sadness at odd times and with unpredictable triggers.
- Disenfranchised Grief: Sadly, this type of grief is so often dismissed and overlooked by society, and sometimes even by the people closest to us. It could be mourning the loss of a pet, an ex-partner, a job, an opportunity, or a miscarriage. The pain is just as real, but the lack of recognition can make the journey to healing much more challenging. People that don’t understand what that thing that was lost meant to you can say things like “just get another one,” further adding to one’s despair.
- Collective Grief: In times of widespread tragedy or national loss, we experience collective grief. It's a shared sorrow that can bring communities together or sometimes drive them apart, as we've seen during global events like the COVID-19 pandemic or the events of 911.
Now, as mentioned earlier on, let's point out a type of grief that often flies under the radar, yet its impact can be profound.
The Silent Burden: Cumulative Grief
Imagine carrying a backpack that gets heavier with each step. Each loss compounding the weight on one’s shoulders. It occurs when multiple losses pile up, often before we've had a chance to process each one individually. This could be a series of deaths in quick succession, or a combination of different types of losses - a job, a relationship, a home.
The danger of cumulative grief lies in its ability to sneak up on us. One might not know they are suffering from it until it’s effects are overwhelming all of a sudden. Each individual loss might seem manageable, but together they can overwhelm our coping mechanisms, leading to a state of emotional exhaustion and despair.
Recognising cumulative grief is crucial for seeking appropriate support and preventing long-term mental health issues. If you find yourself struggling with multiple losses, know that your feelings are valid, and that help is available. You should try not to wait until you feel completely overwhelmed before seeking support.
Seeking Support: Your Path to Healing
When grief threatens to pull you under, reaching out for support can make a world of different in pulling you up to catch your breath and find your way to shore. But where do you start? Here are some avenues to explore:
- Professional Help: Mental health professionals, including therapists and counsellors, are trained to guide you through the grieving process. They can provide coping strategies and a safe space to express your emotions. If you are in the UK, the NHS is equipped to help and provide guidance.
- Support Groups: Sharing your experience with others who are going through grief themselves can be incredibly helpful. Support groups offer understanding, validation, and practical advice. Often times, hearing you are not alone in your struggle can be a powerful catalyst to get you on the road to recovery and management.
- Friends and Family: Don't underestimate the power of your personal support network. Sometimes, a listening ear or a shoulder to cry on can make all the difference.
- Self-Care: While not a replacement for professional help, self-care is crucial in managing grief. This could include:
- Regular exercise to boost mood and reduce stress
- Maintaining a healthy diet to nourish your body and mind
- Getting adequate sleep to help process emotions
- Engaging in relaxation techniques like meditation or yoga.
- Grief Counselling Services: Many organisations offer specialised grief counselling services. These can be particularly helpful if you're dealing with a specific type of loss.
Remember, seeking support is not a sign of weakness. It's a courageous step towards healing and reclaiming your life from the clutches of grief.
Time to Reach Out
As we've journeyed through the landscape of grief, we've seen its many faces and the profound impact it can have on our lives. From the acute sorrow of recent loss to the hidden burden of cumulative grief, each experience is unique and deserving of understanding and support.
Grief is a universal experience, you don't have to face it alone. If you're struggling with any form of grief, or if you're concerned about your mental health in the wake of a loss, it's time to act.
At CAS Medical, we understand the complex interplay between grief and mental health. Our Mental Health Screening service can help you assess your emotional wellbeing and provide guidance on the next steps in your healing journey. Our experienced team is here to listen, understand, and support you through this challenging time.
Don't let grief isolate you. Reach out to CAS Medical today. Together, we can navigate the difficult terrain of loss and find a path to healing. Remember, seeking support is not just a step towards managing your grief - it's an investment in your overall health and wellbeing.
Urticaria: Five Things to Know About Hives
Picture yourself going about your day when suddenly, your skin erupts into a raging itchy rash. This itch can leave you feeling uncomfortable and bewildered. This might get diagnosed as urticaria, more commonly known as hives. While it may not be as debilitating as fibromyalgia, which we've discussed in the previous article, urticaria can still significantly impact your quality of life. Today, we're delving into the itchy, bumpy realm of hives to arm you with knowledge and understanding.
In the next few minutes, we’ll answer five crucial frequently asked questions regarding urticaria that could change the way you view this common yet often misunderstood condition. From its sneaky symptoms to potential dietary triggers, we'll explore the ins and outs of hives, in five minutes or less. But before we dive in, it’s important to note that this is a common condition and there are things that can be done to lessen or eliminate its effects in your life. Did you know that, according to the British Association of Dermatologists, urticaria affects up to 20% of people at some point in their lives? That's right, you're not alone in this itchy battle.
So, without further ado, let's scratch beneath the surface and uncover the five things you need to know about urticaria, aka hives.
1. What exactly is urticaria, and why does it happen?
Like an unwelcome guest, it shows up unexpectedly and causes much discomfort and, sometimes, a feeling of embarrassment. But what's really going on beneath the surface?
At its core, urticaria is an immune reaction, that may be part of a wider allergic response. Your immune system, usually your stalwart defender, suddenly goes into overdrive. It releases a substance called histamine, which causes small blood vessels to leak. The result? Those telltale red, itchy welts we call hives.
But here's where it gets interesting or concerning. Urticaria can be triggered by a veritable smorgasbord of factors:
- Foods (think shellfish, nuts, or eggs). We’ll touch on this some more later in the article.
- Medications
- Insect bites or stings
- Physical stimuli (like pressure or cold)
- Stress (yes, your mind can make you itchy)
- Infections
However, in many cases, the exact cause remains a mystery, making it somewhat tricky to diagnose in some cases.
2. What are the symptoms of hives?
Now, you might be thinking, "Surely, I'd know if I had hives?" Well, not always. Urticaria can be a deceptive, presenting in various ways that might catch you off guard.
The classic symptoms include:
- Welts: Raised, often red bumps on the skin
- Itching: Can range from mild to severe
- Swelling: Particularly in the lips, eyelids, or throat.
But here's where it gets tricky. These symptoms can appear and disappear faster than it can take you to get seen by your doctor making it sometimes more difficult to diagnose. One moment you're itching like mad, the next, your skin looks perfectly normal. This on-again-off-again nature is one of urticaria's hallmarks. Physically being examined by a healthcare provider is crucial for the journey to recovery.
3. Are there different types of urticaria I should be aware of?
Yes. There are different types of urticaria that are commonly experienced. What are they and what differentiates them?
- Acute Urticaria:
- Lasts less than six weeks
- Often triggered by specific allergens or infections
- Usually resolves on its own
- Chronic Urticaria:
- Persists for more than six weeks
- Can last months or even years
- Often has no identifiable cause
- Physical Urticarias:
- Triggered by physical stimuli e.g., dermographism (hives appear when skin is stroked), cold urticaria (triggered by cold temperatures), cholinergic urticaria (brought on by heat or exercise)
Understanding these distinctions is crucial, as they can influence treatment approaches and management strategies.
4. How can I stop urticaria from impacting my daily life?
Living with urticaria can be like trying to navigate a maze blindfolded. The impact on daily life can be unexpected and profound, affecting everything from your wardrobe choices to your social calendar.
Imagine this scenario: You've got an important presentation at work, but you wake up covered in hives. Or perhaps you're planning a romantic evening, only to find your face swollen and itchy. Urticaria doesn't just affect your skin; it can take a toll on your confidence and mental wellbeing too.
But fear not. There are steps you can take to manage its impact:
- Identify and avoid triggers: Keep a diary to track potential causes.
- Dress smart: Opt for loose, cool clothing to minimise irritation.
- Cool it down: Apply cool compresses to soothe itchy areas.
- Stay moisturised: Use fragrance-free, hypoallergenic moisturisers to keep skin hydrated.
- Manage stress: Practice relaxation techniques like meditation or yoga.
Remember, while these self-help measures can provide relief, it's crucial to consult a healthcare professional for proper diagnosis and treatment. They might prescribe antihistamines or other medications to help control symptoms.
5. Can my diet really influence urticaria symptoms?
The relationship between diet and urticaria is like a complex dance - intricate, sometimes unpredictable, but undeniably important.
While food allergies can certainly trigger acute urticaria, the link between diet and chronic urticaria is less straightforward. However, research suggests that what you put on your plate could indeed influence your symptoms.
Certain foods contain naturally occurring histamines or cause the body to release histamine. Foods high in histamine include:
- Fermented foods (think aged cheeses, wine, sauerkraut)
- Cured meats
- Certain fish (particularly if not fresh)
- Spinach and tomatoes
- Chocolate and citrus fruits
But before you clear out your fridge, keep in mind that not everyone with urticaria reacts to these foods.
Some sufferers find relief by following a low-histamine diet, while others get relief from anti-inflammatory foods like omega-3 rich fish, leafy greens, and berries. The key is to work with a healthcare professional or registered dietitian to identify your personal triggers and develop a balanced eating plan that works for you.
Time To Act
Knowledge, as they say, is power. Armed with the information in this blog article, you're better equipped to face the challenge of urticaria head-on. Remember, while hives can be frustrating and uncomfortable, they're not insurmountable.
If you're grappling with persistent or severe urticaria, it's time to take action. Don't let hives control your life. A healthcare professional can provide personalised advice and treatment options tailored to your specific situation.
At CAS Medical, we are here to help you navigate the choppy waters of urticaria. Whether you need help identifying triggers, managing symptoms, or exploring treatment options, we're just a phone call away.
Don't let another day go by feeling uncomfortable in your own skin. Contact CAS Medical today and take the first step towards clearer, calmer skin and a life less itchy.
Fibromyalgia: Unmasking the Invisible Foe
Imagine waking up every morning feeling like you've been hit by a lorry, your body a battlefield of pain and exhaustion. This isn't just a bad day - it's the daily reality for millions living with fibromyalgia, a condition as mysterious as it is debilitating. Like a thief in the night, fibromyalgia steals comfort, energy, and joy.
In this article, we'll peel back the layers of this condition, exploring its impact on body and mind. From unravelling Fibromyalgia symptoms to discovering approaches in chronic pain management, we'll tackle it all. We’ve also included some insights about the fibromyalgia diet that might just be the key to managing this condition better.
What is Fibromyalgia?
This chronic condition is a complex disorder characterised by widespread musculoskeletal pain, often accompanied by a series of other symptoms. According to the NHS, fibromyalgia affects roughly 2-4% of the population, with women being more commonly diagnosed than men. According to an NHS Article on fibromyalgia, some estimates suggest nearly 1 in 20 people may be affected by the condition.
But here's the issue with that statistic - experts believe these numbers might be just the tip of the iceberg, with many cases going undiagnosed or misdiagnosed. A study published in 2010 by BMC Health Services Research found that from the time patients first presented to a doctor for their fibromyalgia symptoms, it took on average 2.3 years and presenting to 3.7 physicians before receiving a diagnosis. Acting fast is critical to getting you closer to a tailored management system quicker.
The exact cause of fibromyalgia largely remains a mystery, but researchers believe it involves a complex interplay of genetic, environmental, and psychological factors. One prevailing theory suggests that fibromyalgia amplifies pain sensations by affecting how the brain and spinal cord process pain signals. It's as if a person’s pain dial has been cranked up very high.
Decoding Fibromyalgia Symptoms
Living with fibromyalgia can feel like being stuck in a never-ending cycle, where symptoms pop up unexpectedly and refuse to stay down. Let's break down some known symptoms:
- Widespread lasting pain: Widespread pain lasting at least three months is a characteristic of fibromyalgia. It's not just a bit of discomfort, but pain that can make you feel unforgivingly overexerted.
- Fatigue: Even after a full night's sleep, people with fibromyalgia often wake up feeling as exhausted as when they haven’t had any sleep. It's like trying to fill a leaky bucket - no matter how much rest you get, it never seems to be enough.
- Cognitive difficulties aka 'fibro fog': This cognitive dysfunction can make concentrating very challenging.
- Mood swings: Anxiety and depression often accompany fibromyalgia, greatly upsetting one’s emotional stability.
- Headaches and migraines: Tension headaches and full-blown migraines are a common complaint amongst fibromyalgia sufferers.
- Digestive issues: Digestive issues, such as irritable bowel syndrome (IBS) can also often rear its head.
- Sensory overload: Many people with fibromyalgia find themselves more sensitive, reacting strongly to temperature, light, or sound.
Chronic Pain Management Strategies
Now, don't lose all hope - while fibromyalgia might be debilitating and tough to deal with, there are ways to manage this chronic condition better.
- Get moving: Regular, gentle exercise can help reduce pain and improve overall well-being. A bit of swimming, yoga, or tai chi can work wonders.
- Sleep hygiene: Establishing a sleep routine that's as regular and coordinated as work meeting times can improve sleep quality and reduce fatigue. Create a bedroom environment that if purposeful for sleep and tailored to conditions that best induce sleep for you. There are lots of helpful strategies that you can try. Here’s a helpful article by the Sleep Foundation - Bedroom Environment: What Elements Are Important?
- Stress management: This is often easier said than done because we worry and stress over the things we worry and stress over for good reasons, especially if that reason is chronic pain. But techniques like mindfulness meditation, deep breathing exercises, or cognitive-behavioural therapy can help you manage stress and anxiety.
- Therapeutic approaches: Heat therapy, gentle massage, or acupuncture might provide relief for some individuals. Discuss this with your healthcare provider first to explore what’s safe, accessible, and works for you.
- Medication: Your healthcare provider might prescribe various medications to manage pain, improve sleep, or address associated symptoms. Remember though, medication is just one tool in your fibromyalgia-fighting toolkit. A concerted effort in a multi-pronged strategy might be needed to effectively manage fibromyalgia.
Fueling the Fight: The Fibromyalgia Diet
While there's no magic ‘fibromyalgia diet’, certain nutritional approaches might help to alleviate symptoms.
| Foods to Include | Foods to Limit |
| Anti-inflammatory foods (e.g., fatty fish, berries, leafy greens) | Processed foods |
| Whole grains | Refined sugars |
| Lean proteins | Excessive caffeine |
| Hydrating beverages | Alcohol |
Some individuals with fibromyalgia report benefits from following some well-known diets, such as:
Dietary changes should be discussed with a healthcare professional or registered dietitian to ensure you're not throwing the baby out with the bathwater when it comes to nutrition. It is important that your nutritional needs are met.
Speak to us about a personalised wellness plan. Click the image below
Mind Over Matter: The Mental Health Connection
Living with fibromyalgia can be as mentally taxing as it is physically challenging. It can take a toll on mental health, with many individuals experiencing anxiety, depression, or mood changes. Addressing these aspects is crucial for overall well-being.
- Seek support: Connect with support groups or online communities. After all, a problem shared is a problem halved. The NHS provide access to related services. With CAS Medical, you can skip the often-long waiting times and access private healthcare specialists a lot quicker and put yourself in the driver’s seat to fibromyalgia management.
- Prioritise self-care: Engage in activities that bring joy and relaxation. Discover new ones with loved ones, like-minded individuals or others in your support network.
- Consider therapy: Cognitive-behavioural therapy or other forms of counselling can help manage the emotional impact of fibromyalgia.
The Light at the End of the Tunnel: Research and Hope
Scientists and other experts are working tirelessly to unravel the mysteries of this condition, with promising research in areas such as:
- Neuroimaging studies to better understand pain processing in the brain
- Genetic research to identify potential risk factors
- Investigating the role of the gut microbiome in fibromyalgia symptoms
- Exploring novel treatment approaches, such as transcranial magnetic stimulation
Empowering Yourself: Take Charge Today
Living with fibromyalgia is no walk in the park, but armed with knowledge and determination, you can face this condition head-on. But you must act. Remember, you're not just a passenger in this journey – no one else can feel exactly what you feel so taking the necessary steps towards a better quality of life is critical.
Educate yourself, communicate openly with your healthcare team, and build a strong support network. Keep a symptom journal to identify triggers and patterns, and be patient with yourself – it is a marathon, not a sprint. Don’t jump into health fads and the latest health craze you see online so you don’t invertedly make things worse, delay your recovery, or develop other conditions.
By taking an active role in your health and well-being, you can develop strategies to manage fibromyalgia and improve your quality of life. Remember, even on the darkest days, there's always a glimmer of hope.
If you feel you or someone you know might be experiencing symptoms that are similar to those mentioned above, don’t delay, speak to us today. Start your journey towards a diagnosis and management plan now for a better quality of life.
Contact Form: https://www.casmedical.org/contact/
Phone us: 0141 280 6956
We operate clinic days in Bothwell, Glasgow, and Stirling. Contact us to book an appointment.
Erectile Dysfunction Help: Causes and Treatment Options
Erectile dysfunction (ED) affects millions of men in the UK. Contrary to common notions about this condition, it doesn't just affect older men - it can hit at any age due to physical or psychological reasons. The impact on relationships and self-esteem can be significant.
Understanding likely causes and available treatment options is crucial for eliminating the stigma around the condition, provide solutions, and boost confidence in seeking professional help. From the latest treatments to lifestyle changes, there are numerous approaches to help address erectile dysfunction effectively.
Whether it's exploring medical interventions, considering the role of certain medications, or looking into the connection between ED and conditions like diabetes, this article aims to provide a comprehensive overview. You will gain valuable insights to help you make informed decisions about your penile health and well-being.
Understanding Erectile Dysfunction
Definition and Prevalence
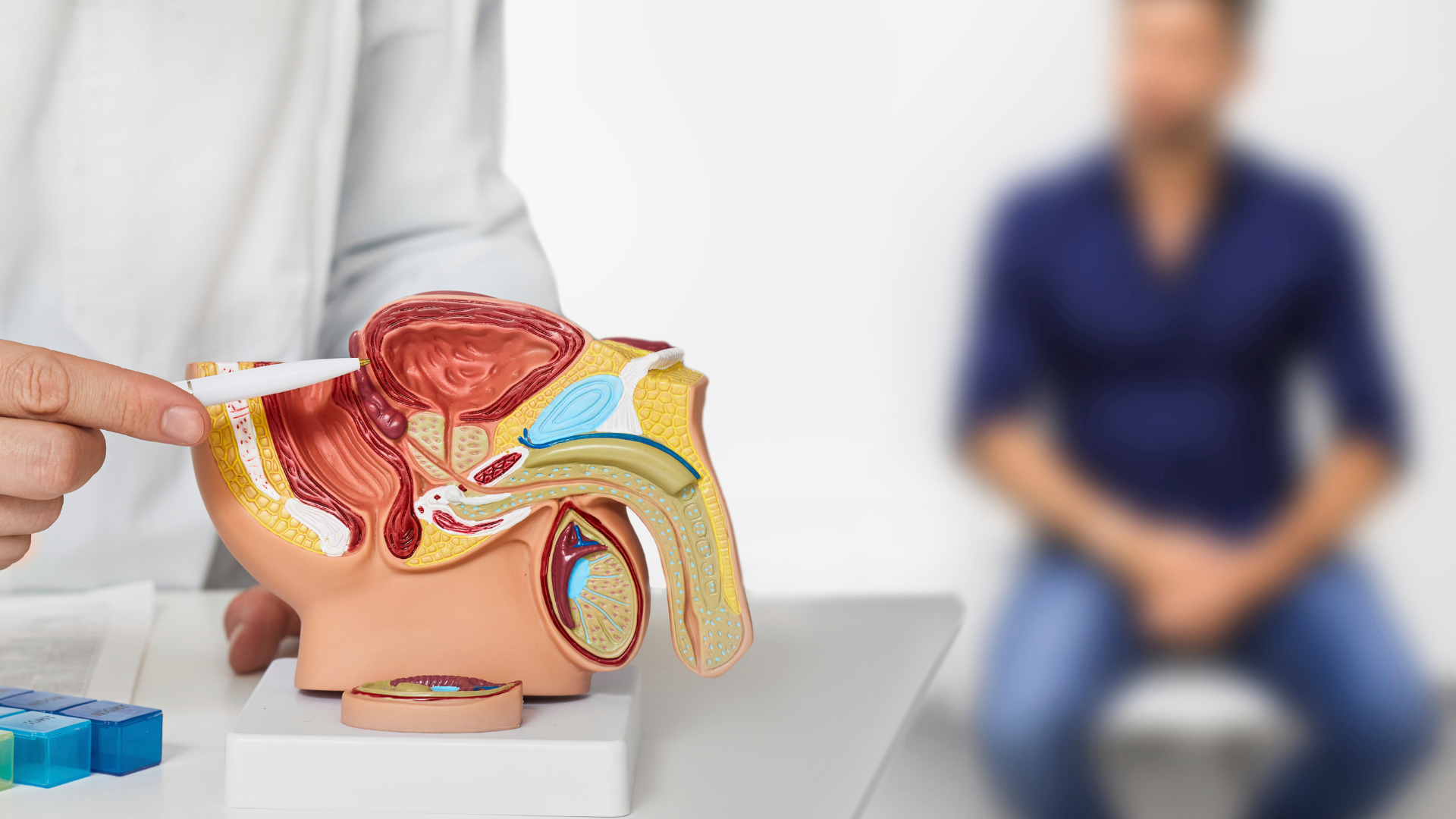
When stimulated, the nerves release chemicals that increase blood flow to the penis. Blood flows into two erectile chambers in the penis that are made of spongy muscle tissue (cavernosoma). During arousal, the spongy tissue relaxes and traps blood. The blood pressure in the chambers cause the penis to become firm causing an erection. When a man reaches orgasm, other nerve signals reach the penis, the muscle tissue in the penis relaxes, and blood is pumped back into the man's circulation, causing the erection to decrease. A regular disruption to this process can cause erectile dysfunction which leads to a persistent inability to achieve or maintain a penile erection sufficient for satisfactory sexual performance.
According to the Massachusetts Male Aging Study, the total prevalence of ED among men aged 40-70 years was 52 percent, although it also affects younger men. Globally, it was estimated that over 152 million men experienced ED in 1995. It is now projected that this number could rise to approximately 322 million by 2025.
Common Causes of Erectile Dysfunction
Erectile dysfunction is a complex condition with various possible underlying causes. Mayo Clinic outline that physical issues such as heart disease, high cholesterol, high blood pressure, diabetes, and obesity can lead to ED. Additionally, psychological factors like depression, anxiety, stress, and relationship problems can interfere with sexual function. Often, it's a combination of both physical and psychological factors.
Endothelial dysfunction is a common pathway in many cases of erectile dysfunction. Endothelial dysfunction is a type of non-obstructive coronary artery disease (CAD) in which there are no heart artery blockages, but the large blood vessels on the heart's surface narrow instead of dilating. This condition can affect the blood vessels and nerves essential for achieving and maintaining an erection. Other potential causes include neurological diseases, hormonal imbalances, and the use of certain medications.
Risk Factors of Erectile Dysfunction
Several risk factors contribute to the development of ED:
- Age: The risk of erectile dysfunction increases with age, with about 40% of men affected at age 40 and 70% by age 70.
- Chronic diseases: Conditions such as diabetes, cardiovascular disease, and chronic kidney disease can significantly increase the risk of ED.
- Lifestyle factors: Smoking, excessive alcohol consumption, lack of physical activity, and being overweight can also contribute to erectile dysfunction.
- Medications: Certain drugs, including some blood pressure medications, antidepressants, and prostate cancer treatments, can have ED as a side effect.
- Psychological factors: Stress, anxiety, depression, and low self-esteem can all play a role in the development of erectile dysfunction.
Understanding these aspects of ED is crucial for men experiencing this condition. It's important to remember that it is a common and treatable issue, and seeking professional help can lead to effective management and improved quality of life.
Diagnosing Erectile Dysfunction
Medical History and Physical Exam
The diagnostic process for erectile dysfunction begins with a comprehensive medical and sexual history, followed by a physical examination. Doctors typically ask questions about the onset, context, and frequency of ED symptoms.
They also inquire about lifestyle factors, general health, and any medications the patient is taking. A physical exam includes checking blood pressure, assessing body mass index, and a genital examination. This initial assessment helps differentiate between physical and psychological causes of ED.
At CAS Medical, we take extra measures to ensure that we create a safe and open environment When possible, including the partner in the assessment can provide valuable insights, as they may be aware of issues the patient has overlooked or suppressed.
Medical Treatments for Erectile Dysfunction
Medications
Oral medications are often the first line of treatment. These medications, known as PDE5 inhibitors, enhance the effects of nitric oxide, a chemical that relaxes muscles in the penis, boosting blood flow and helping to achieve an erection.
For patients who don't respond well to oral medications, other effective forms of treatment are available. These include Intracavernosal (injectable), intraurethral (squirted down the opening of the penis) or topical applications. The injectable form causes an erection firm enough for sex in more than 80% of men with ED, according to WebMD.
Penis pumps and implants may be deemed suitable by a urologist.
Testosterone Replacement Therapy
Testosterone Replacement Therapy (TRT) can be beneficial for men with low testosterone levels and mild ED. Studies have shown that TRT improves erectile function in men with low testosterone, with greater improvements observed in studies using a lower testosterone threshold. TRT has also demonstrated consistent benefits in improving libido in men with low testosterone levels.
It's important to note that these treatments should only be used under medical supervision. Patients should discuss potential side effects and contraindications with their healthcare provider to determine the most suitable treatment option for their individual needs.
In cases where a patient fails to respond to oral therapy of topical therapies, we can help with referrals to urology specialists.
Lifestyle Changes and Alternative Therapies
Diet and Exercise
A healthy diet and regular exercise have a significant impact on erectile function. Dietary improvements help with blood flow, crucial for achieving and maintaining erections. Weight loss can also improve erectile dysfunction in overweight or obese individuals.
Regular physical activity is equally important. Moderate to high levels of exercise are associated with a lower risk of ED [National Library of medicine - Lifestyle modifications and erectile dysfunction: what can be expected?]. According to this research paper, 150 minutes of weekly aerobic activity for three months can lead to improved erectile function and reduced markers of endothelial dysfunction.
Stress Management
Stress can significantly interfere with sexual function and cause erectile dysfunction. Implementing stress management techniques can help improve erectile function. One study showed that an eight-week stress management program, including diaphragmatic breathing exercises and progressive muscle relaxation, lead to significant improvements in perceived stress and erectile function scores.
Natural Remedies
Some natural remedies have shown promise in managing ED. However, it's important to note that the effectiveness of these remedies varies, and more research is needed to confirm their benefits.
Take Action Today
Erectile dysfunction is a complex issue that affects many men, with a range of possible causes but with treatment options available. From oral medications to lifestyle changes, there are numerous ways to address this condition and improve quality of life.
Understanding the root causes, seeking proper diagnosis, and exploring the various treatment options are key steps in addressing the condition effectively. By taking a holistic approach that includes medical interventions, dietary adjustments, and stress management techniques, many men can find relief and regain confidence in their sexual health.
For those grappling with erectile dysfunction, it's important to remember that help is available. Contact CAS Medical for discrete, personalised guidance and treatment plans tailored to your individual needs.
Rosacea: Causes, Symptoms, and Management
Rosacea is a chronic skin condition that affects millions of people in the UK, particularly those with fair skin. This article will provide a comprehensive overview of rosacea, including its causes, symptoms, and management strategies. We'll explore various treatment options and preventative approaches to help you better understand and control this often-misunderstood condition.
In this article, you'll learn:
- What rosacea is and who it typically affects
- The main symptoms and triggers of rosacea
- Effective treatment options and preventative measures
- How to manage rosacea in your daily life
Understanding Rosacea: Causes and Symptoms
What is Rosacea?
Rosacea is a chronic inflammatory skin condition that primarily affects the face. It's characterised by redness, visible blood vessels, and sometimes small, pus-filled bumps. While it can affect anyone, rosacea is most common in fair-skinned individuals of Northern European descent.
According to the National Rosacea Society, an estimated 415 million people worldwide are affected by rosacea. In the UK, it's believed that up to 1 in 10 people may have some form of rosacea, though many cases go undiagnosed.
Symptoms of Rosacea
The primary symptoms of rosacea include:
- Facial redness (erythema): Persistent redness in the central part of the face.
- Visible blood vessels (telangiectasia): Small blood vessels on the nose and cheeks become visible.
- Swollen red bumps: Some people develop small, red, pus-filled bumps that may resemble acne.
- Eye problems: In some cases, rosacea can affect the eyes, causing dryness, irritation, and swollen eyelids.
- Enlarged nose: In severe cases, the skin on the nose may thicken, leading to a condition called rhinophyma.
Causes and Triggers
While the exact cause of rosacea remains unknown, researchers believe it involves a combination of genetic and environmental factors. Some common triggers include:
- Exposure to sunlight
- Extreme temperatures (hot or cold)
- Spicy foods and hot drinks
- Alcohol consumption
- Stress and anxiety
- Certain skincare products
- Exercise
- Some medications
It's important to note that triggers can vary from person to person. Keeping a diary of flare-ups can help identify your specific triggers.
Managing Rosacea: Treatment Options and Preventative Approaches
Treatment Options
While there's no cure for rosacea, various treatments can help manage symptoms and reduce flare-ups. Treatment options include:
- Topical medications: Creams or gels containing ingredients like metronidazole, azelaic acid, or ivermectin can help reduce redness and inflammation.
- Oral antibiotics: For more severe cases, oral antibiotics like doxycycline may be prescribed to control inflammation.
- Laser and light therapies: These treatments can help reduce visible blood vessels and overall redness.
- Skincare routines: Gentle, non-irritating skincare products can help soothe and protect rosacea-prone skin.
- Lifestyle changes: Identifying and avoiding triggers can significantly reduce flare-ups.
Preventative Approaches
While it's not always possible to prevent rosacea, there are steps you can take to minimise flare-ups and protect your skin:
- Sun protection: Use a broad-spectrum sunscreen with at least SPF 30 daily, even on cloudy days.
- Gentle skincare: Choose fragrance-free, non-comedogenic products designed for sensitive skin.
- Avoid known triggers: Once you've identified your triggers, take steps to avoid or minimise exposure to them.
- Stress management: Practice stress-reduction techniques like meditation or yoga to help prevent stress-induced flare-ups.
- Diet modifications: Consider reducing your intake of spicy foods, hot drinks, and alcohol if these trigger your symptoms.
- Temperature regulation: Protect your face from extreme temperatures, both hot and cold.
Management and Control
Living with rosacea can be challenging, but with the right knowledge and management strategies, it's possible to control symptoms and improve your quality of life. Remember that rosacea is a chronic condition, and consistent care is key to managing it effectively.
Key takeaways:
- Rosacea is a common skin condition affecting millions in the UK
- Symptoms include facial redness, visible blood vessels, and sometimes bumps or eye problems
- While there's no cure, various treatment options can help manage symptoms
- Identifying and avoiding triggers is crucial for preventing flare-ups
- Consistent skincare and lifestyle modifications can significantly improve rosacea management
If you suspect you have rosacea or are struggling to manage your symptoms, don't hesitate to contact us. We can help identify the condition and get you the help you need.
Staying Healthy During Your Summer Holidays Abroad
As the summer of 2024 approaches, many Scots are eagerly planning their holidays abroad. While the excitement of exploring new destinations is palpable, it's crucial to prioritise staying healthy during your travels. This guide will equip you with practical strategies for staying healthy on your summer holidays, ensuring you make the most of your well-deserved break.
In this post, you'll learn:
- Essential preventative health measures before you travel
- Tips for maintaining your wellbeing whilst abroad
- How to handle common health issues that may arise on holiday
Let's dive in and set you up for a healthy and enjoyable summer adventure.
1. Pre-Travel Health Preparations
Before you jet off to sunnier climes, a bit of preparation can go a long way to staying healthy.
Get Your Jabs Sorted
First things first, check if you need any vaccinations for your destination. Don't leave this to the last minute – some vaccines need to be administered weeks before travel.
Pack a Personal Health Kit
Assemble a small health kit tailored to your needs. Include:
- Any regular medications (pack extra in case of delays)
- Painkillers
- Plasters and antiseptic wipes
- Insect repellent
- Sun cream (at least SPF 30)
- Rehydration sachets
You don’t want to be that one that’s arrived the paradise destination and turned it to a nightmare because you’ve forgotten to pack a well-stocked health kit that can save your holiday. Mom’s across the world have always been the champions of holidays. You can’t be overprepared, only underprepared.
Travel Insurance: Don't Leave Home Without It
While it might seem like an unnecessary expense, comprehensive travel insurance can be a lifesaver. Make sure it covers any pre-existing conditions and activities you plan to do on holiday.
2. Staying Healthy While Abroad
Now that you're prepared, let's look at how to maintain your health during your summer holidays.
Stay Hydrated, Stay Happy
It's easy to become dehydrated in hot climates, especially if you're more active than usual. Aim to drink at least 2 litres of water a day. If you're unsure about the local water quality, stick to bottled water.
Mind What You Eat
Trying local cuisine is one of the joys of travel, but be mindful of food safety. A study in the National Library of Medicine speaks of “Travellers' diarrhoea.” It affects up to 50% of those visiting developing countries. It is primarily caused by various organisms, with enterotoxigenic Escherichia coli being the main culprit. Travellers can reduce their risk by eating and drinking cautiously. Additionally, they should have a rehydration and treatment plan ready to minimise the illness's impact.
To reduce your risk:
- Opt for freshly cooked, hot foods
- Avoid raw or undercooked meats and seafood
- Be cautious with street food – choose vendors with high turnover and good hygiene practices
- Peel fruits yourself or stick to fruits with thick skins
Keep Moving
While holidays are for relaxation, maintaining some level of physical activity can boost your mood and health. Consider:
- Morning beach walks
- Swimming in the hotel pool
- Exploring your destination on foot
Remember, every little bit of movement counts.
However, be very cautious when swimming in public swimming pools when on holiday as standards for cleaning public pools can be very different from what applies in the UK. Sometimes the pools aren’t cleaned as often or well, and sometimes too much cleaning agents are used. A recent patient of ours suffered from irritable eyes for 10 years from one holiday in 2014.
3. Handling Common Holiday Health Issues
Even with the best preparations, health niggles can occur. Here's how to handle some common issues:
Sunburn: Prevention and Treatment
Despite our familiarity with rainy Scottish weather, many of us still fall victim to sunburn abroad. To avoid this:
- Apply sunscreen generously and frequently
- Seek shade during the hottest part of the day (usually 11am-3pm)
- Wear protective clothing, including a wide-brimmed hat
If you do get burned, cool the skin with damp cloths and apply after-sun lotion. Stay hydrated and out of the sun until your skin heals.
A common skin condition that we see is Pityriasis Versicolor, uneven patches skin changing colour in the sun. It can occur due to increased heat and humidity.
Dealing with Digestive Troubles
If you experience travellers' diarrhoea:
- Stay hydrated with bottled water or oral rehydration solutions
- Eat bland, easily digestible foods
- Consider taking over-the-counter anti-diarrhoeal medication for short-term relief
Be sure to check medications purchased abroad for authenticity. Often times, a Google search of the product can alert you to certain red flags for that drug. Be careful. Seek professional medical advice from an accredited healthcare provider before taking medications.
If symptoms persist for more than a few days or are accompanied by fever, seek further medical attention.
Jet Lag: Minimising the Impact
Travelling across time zones can wreak havoc on your sleep patterns. To minimise jet lag:
- Adjust your sleep schedule a few days before travel
- Staying hydrated during your flight is important for staying healthy
- Try to stay awake until the local bedtime at your destination
Ready, Prepped, Go
Staying healthy during your summer holidays doesn't have to be a chore. With a bit of preparation and mindfulness, you can enjoy your time abroad to the fullest. Remember to:
- Prepare adequately before you travel
- Research common local health issues and prepare accordingly
- Stay hydrated and eat mindfully
- Keep active, but listen to your body
- Know how to handle common health issues
By following these guidelines, you're setting yourself up for a fantastic, healthy holiday. So go ahead, book that trip, and create some unforgettable memories.
Insomnia Help: From Sleep Hygiene to New Medical Options
Insomnia is a prevalent sleep disorder affecting millions worldwide. It is characterised by difficulty falling asleep, staying asleep, or both, despite having adequate opportunity for rest. This article aims to provide comprehensive information about insomnia, its impacts, and various management strategies you can use to take back control of your rest time.
Understanding Insomnia
Insomnia is more than occasional sleeplessness. It's a persistent condition that can significantly impair one's quality of life. Acute insomnia may last from a few days to weeks, while chronic insomnia persists for months or even years. Recognising the difference is crucial for seeking appropriate help. Many people experience short-term sleep difficulties due to stress, travel, or life changes. However, when sleep problems become a more regular occurrence, it may be time to consider whether you're dealing with insomnia.
The Far-Reaching Impact of Insomnia
The effects of insomnia extend far beyond night time discomfort. It often leads to profound consequences on various aspects of daily life:
Decreased Work Performance:
Insomnia can have a significant negative impact on productivity and concentration at work. This can in a lot of cases lead to potential career setbacks as you might find yourself struggling to complete tasks that were once easy, or making mistakes you wouldn't normally make. Simple projects become difficult projects with delays and worse, a lack of trust in the quality of your own work. It’s important to speak out when you start noticing these problems.
Increased Accident Risk:
Fatigue from insomnia can impair judgment and reaction times, raising safety concerns. This is particularly dangerous if you drive or operate machinery regularly.
Mental Health Implications:
Chronic sleep deprivation may contribute to mood disorders, including depression and anxiety. It's a vicious cycle - lack of sleep can worsen mental health, and poor mental health can make it harder to sleep.
Cognitive Function Decline:
Memory, decision-making, and problem-solving abilities can be significantly affected. Insomnia sufferers often find themselves forgetting important details or struggling to focus during important meetings. Ever find yourself lost as to what you came into a room to find? Or forgetting a close friend’s name? Cognitive decline can stem from a number of health reasons. Rule out insomnia as best you can by taking action against it today.
Physical Health:
Insomnia can weaken the immune system, thereby considerably increasing your susceptibility to various serious health issues. Some studies have linked chronic insomnia to an increased risk of cardiovascular problems and diabetes. Your body needs sleep. It needs ample rest. Even the best machine needs to shut down and reset periodically to maintain optimal functionality and your body is no different. Ideally, night time rest should be between seven and eight hours of sleep. Some people don’t sleep at all while some others only manage three or four hours of sleep.
Relationship Strain:
Increased irritability and negative mood changes can negatively impact one’s personal and professional relationships. You might find yourself snapping at loved ones or withdrawing from social activities irrationally and without clear triggers.
Insomnia and Absenteeism
A study published in the National Library of Medicine [Link] found varying degrees of insomnia in 79.9% of the study population. In the study, 57.2% experienced mild insomnia, 21.4% had moderate insomnia, and 1.3% suffered from severe insomnia. Insomnia was more common among those frequently absent from work or leaving due to illness. Those with moderate to severe insomnia had significantly higher total absenteeism compared to those with mild or no insomnia.
Non-Pharmacological Approaches: Sleep Hygiene and Lifestyle Changes
Before considering medication, it's essential to explore non-drug options for managing insomnia. Good sleep hygiene practices can make a significant difference in your sleep quality.
- Maintain a Consistent Sleep Schedule: Regulate your body's internal clock by going to bed and waking up at the same time daily, including weekends. This helps train your body to expect sleep at certain times.
- Create a Relaxing Bedtime Routine: Engage in calming activities like reading or gentle stretching before bed. This signals to your body that it's time to wind down.
- Optimise Your Sleep Environment: Ensure your bedroom is dark, quiet, and cool for optimal sleep conditions. Consider using blackout curtains, earplugs, or a white noise machine if needed.
- Diet and Exercise: Avoid caffeine, alcohol, and large meals close to bedtime. Regular exercise can promote better sleep, but not too close to bedtime.
- Stress Management: Practice relaxation techniques such as meditation, deep breathing exercises, or progressive muscle relaxation. These can help quiet a racing mind and prepare your body for sleep.
- Limit Screen Time: This one is very important. Reduce exposure to blue light from electronic devices at least an hour before bedtime. The blue light can interfere with your body's production of melatonin, the ‘sleep hormone, as it regulates sleep.
Traditional Short-Term Pharmacological Options
In some cases, healthcare providers may prescribe short-term medication to address acute insomnia. Non-benzodiazepine hypnotics are commonly prescribed.
These medications are typically recommended for short durations. Usually up to 4 weeks. It is crucial that you use these under medical supervision due to potential side effects and the risk of dependence.
Emerging Long-Term Pharmacological Options
Recent advancements in sleep medicine have led to the development of a new class of medications. This new category, known as 'orexin receptor antagonists', targets the brain's wake-promoting system.
These medications may be suitable for longer-term use in some patients, under careful medical supervision. As with any medication, it's essential to discuss potential benefits and risks with a healthcare provider first.
When to Seek Professional Help
If insomnia persists despite implementing sleep hygiene practices, consult a healthcare professional as soon as possible. But how do you know when it's time to seek help? Here are some signs that indicate it might be time to consult a sleep specialist:
- Your sleep problems persist for more than a month.
- Insomnia is significantly affecting your daily life, work performance, or relationships.
- You're relying on over-the-counter sleep aids or alcohol to fall asleep.
- You experience symptoms of other sleep disorders, such as loud snoring or gasping for air during sleep.
- You feel anxious or frustrated about your sleep, which makes it even harder to fall asleep.
At CAS Medical, we offer comprehensive sleep assessments. These assessments involve a detailed discussion of your sleep patterns, lifestyle factors, and overall health. We may also recommend a sleep study, which can provide valuable insights into your sleep architecture and identify any underlying sleep disorders.
Based on the results, we develop personalised treatment plans that may include a combination of cognitive behavioural therapy for insomnia (CBT-I), lifestyle modifications, and, if necessary, appropriate medication. Our goal is to help you achieve restful, restorative sleep without relying on long-term medication use when possible.
If required, you can get faster access to see sleep specialists through our network of private healthcare providers.
Cognitive Behavioural Therapy for Insomnia (CBT-I)
CBT-I is a structured program that helps identify and replace thoughts and behaviours that cause or worsen sleep problems with habits that promote sound sleep. This non-pharmacological approach has shown significant effectiveness in treating chronic insomnia.
CBT-I typically involves several components:
- Sleep restriction therapy to improve your sleep efficiency
- Stimulus control therapy to associate your bed with sleep
- Relaxation training to reduce physical tension
- Cognitive therapy to challenge unhelpful thoughts about sleep.
Take Action
Insomnia can be a challenging condition, but effective management options are available. From improving sleep hygiene to exploring new medical treatments, there are numerous paths to better sleep. If you're struggling with persistent sleep issues, don't hesitate to reach out to us for professional help.
Remember, quality sleep is fundamental to overall health and well-being. Taking steps to address insomnia can lead to significant improvements in your daily life and long-term health.
For those experiencing sleep-related breathing issues, such as snoring or pauses in breathing during sleep, it may be worth exploring the possibility that you have sleep apnoea. Click the link to learn more about this condition in our article on understanding sleep apnoea.
Don't let insomnia control your life. Reach out to us today, and let's work together towards better sleep and a healthier you. Contact CAS Medical to discuss your sleep concerns and explore personalised solutions.